|
Case Report
Infantile hemangioma: Case report
1 Department of Pathological Anatomy, Mohammed V Military Training Hospital, Faculty of Medicine and Pharmacy, Mohamed V University in Rabat, Rabat, Morocco
Address correspondence to:
Dounia Benaich
Department of Pathological Anatomy, Mohammed V Military Training Hospital, Faculty of Medicine and Pharmacy, Mohamed V University in Rabat, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100014P03JA2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Benaich D, Benbella L, Azekhmam M, Elouchi MR, Elktaibi A, Allaoui M, Chahdi H, Damiri A, Essaoudi MA, Oukabli M. Infantile hemangioma: Case report. Edorium J Pathol 2025;9(1):6–9.ABSTRACT
Introduction: Infantile hemangioma (IH) is a benign vascular tumor with an estimated prevalence of around 10% in children under one year of age.
Case Report: In this case, we describe the case of a 4-month-old girl with a known Beckwith–Wiedemann syndrome. Clinical examination revealed an axillary nodule, initially suspicious of tuberculosis. A skin biopsy confirmed the diagnosis of IH.
Conclusion: Infantile hemangiomas are benign vascular tumors that occur in infants. They typically appear shortly after birth, grow rapidly during the first few months. Histopathological analysis remains essential in cases where the clinical appearance is atypical.
Keywords: GLUT1, Infantile hemangioma, Propranolol, Vascular tumor
INTRODUCTION
Infantile hemangioma (IH) is a benign vascular tumor with an estimated prevalence of around 10% in children under one year of age [1]. In typical forms, diagnosis is easy and based on clinical features. On other cases, the diagnosis can be challenging; thus, histological examination with sometimes a panel of immunohistochemistry are necessary. When the anamnesis or clinical findings are not suggestive, the first-line complementary examination is a Doppler ultrasound performed by an experienced radiologist. The tumor appears hypervascularized, with low-resistance intratumoral arterial flow [2],[3]. Finally, the objective of this work is to describe the clinical, histological, and immunohistochemical characteristics of this tumor. We report a rare case of IH, the diagnosis of which was confirmed by histopathological examination.
CASE REPORT
In this case, we describe the case of a 4-month-old girl with a known Beckwith–Wiedemann syndrome. Clinical examination revealed an axillary superficial nodule, initially suspicious of tuberculosis. Ultrasound of the soft tissue showed a vascular appearance and hyperemia on Doppler. A skin biopsy confirmed the diagnosis of IH.
In most cases, clinical and radiological features are enough for the diagnosis, while in more atypical presentations the microscopic examination is necessary.
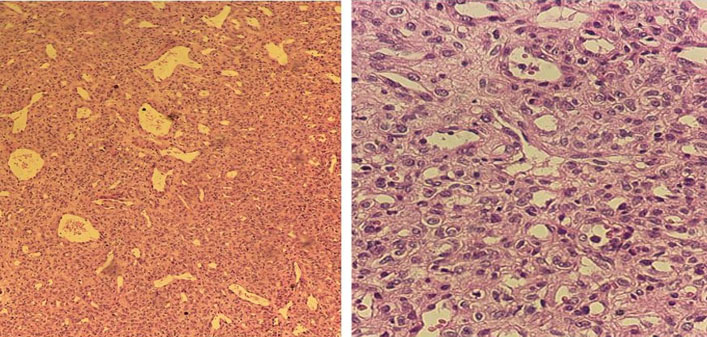
Histologically, it is a benign, well-limited tumor proliferation made up of more or less spindle-shaped cells arranged in nests, devoid of cytonuclear atypia and delimiting vascular slits with a narrow lumen, lined by regular endothelial cells. No histological evidence of malignancy was noted (Figure 1A and Figure 1B).
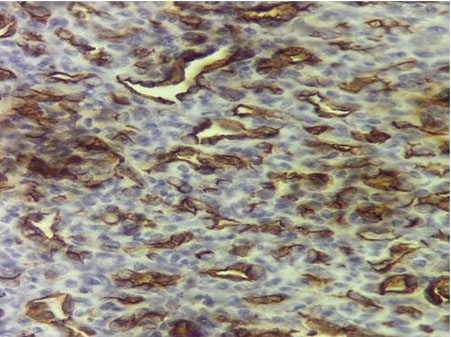
Immunohistochemical analysis showed intense expression of human glucose transporter protein-1 (GLUT-1) by the endothelial cells (Figure 2). Treatment with oral propranolol was introduced at a dose of 1 mg/kg/d, and after three months the hemangioma began to shrink.
DISCUSSION
Infantile hemangioma is a benign, soft tissue tumor of infancy with a reported incidence of 5–10% [4]. The precise incidence of IH is difficult to ascertain as other vascular anomalies had been misclassified under IH’s nomenclature prior to improvements in diagnostic criteria and capabilities. Morphologic variation in hemangioma lesions has muddled this distinction as well. Differential diagnosis includes congenital hemangiomas (non-involuting congenital hemangioma, or NICH, and rapidly involuting congenital hemangioma, or RICH), which can be distinguished from IH by their presence at birth. Furthermore, congenital hemangiomas do not grow postnatally. Congenital hemangiomas can be detected by prenatal ultrasound and do not stain with the immunohistochemical marker, glucose transporter-1 (GLUT-1) [4],[5]. Various demographic studies have revealed many insights into IHs. The tumor occurs at a higher frequency in female infants and ethnic predilection for Caucasian infants is also well known [5],[6]. Additional associated risk factors include low birth weight, prematurity, and products of multiple gestation [6],[7]. Prenatal risk factors found to be linked to IH include advanced maternal age, pre-eclampsia, and placenta previa [6].
Infantile hemangiomas begin to appear during the first few weeks of life either as a telangiectatic patch or an area of pallor. The evolution of IH varies and can either change into small, bright red lesions or large, bulky tumors. The heterogeneous nature of IHs is often described by three clinical morphologies: (1) superficial; (2) deep; and (3) mixed [5],[8],[9]. Superficial hemangiomas present with a bright red color and are located at the superficial dermis. Deep hemangiomas involve the deep dermis and subcutis and appear as blue or skin-colored nodules. Mixed hemangiomas have components of both superficial and deep IHs.
Diagnosis is made primarily based on clinical characteristics and biologic behavior as already described while histologic diagnosis is currently the gold standard. The histopathologic features of IH vary depending on the stage of the IH. Initially, rapidly proliferating, plump, endothelial-like cells and pericytes are present. Vascular lumens begin to appear during the early proliferative phase. Later during the proliferating phase, fibrous septae containing large vessels separate lobules of plump endothelial-like cells. Mitotic figures, apoptotic bodies, and mast cells may also be present within the IH. Finally, during the involutional phase, flattening of the endothelial-like cells, reduction in mitotic figures, decrease in vessels, and appearance of fibrofatty tissue are noted [10].
Anatomopathology remains an essential diagnostic tool for confirming the benign nature of IHs and ruling out other diagnosis.
Immunohistochemically, positive staining of endothelial cells in IH tumor specimens with GLUT-1, present at all stages, can differentiate IH from other vascular tumors and malformations [11]. The immunodiagnostic marker, GLUT-1, has been useful in differentiating IH from other vascular anomalies such as congenital hemangiomas, which are present at birth and will not stain with GLUT-1.
Although IHs have a benign evolution, one study found a 24% complication rate, with 38% of IH infants receiving therapy [12]. As the authors note, these infants were seen at referral pediatric dermatology centers, most likely overestimating the complication rate and need for treatment found in the study. Complications include ulceration, bleeding, infection, visceral involvement, obstruction of the airway, visual compromise, and disfigurement and can result in a significant amount of morbidity.
Treatment for IH may be necessary to prevent or improve functional impairment or pain, prevent or improve scarring or disfigurement, and avoid life-threatening complications. Accepted treatments include intralesional and systemic corticosteroids, chemotherapy (vincristine and interferon alpha), liquid nitrogen cryotherapy, laser ablation, and surgical excision [13]. Corticosteroids are currently the preferred therapy for most types of IH.
Recent interest in the use of propranolol in the treatment of IH followed a 2008 report by Leìauteì-LabreÌze following an incidental finding [14]. Following several corroborative reports, propranolol therapy was further investigated in a twenty-patient randomized control trial (RCT) [15].
CONCLUSION
Infantile hemangiomas are common benign vascular tumors in infants. They typically appear shortly after birth, grow rapidly during the first few months.
Histopathological analysis remains essential in cases where the clinical appearance is atypical. Microscopical findings are important to distinguish infantile hemangioma from other vascular tumors or malignant lesions, thus guaranteeing appropriate treatment and management.
REFERENCES
1.
Berton M, Maruani A. Anomalies vasculaires superficielles (angiomes). EMC - Pédiatrie 2014;9(4):1–11. [CrossRef]

2.
Eschard C. Infantile haemangioma: When investigation is necessary and current therapeutic developments. [Article in French]. Ann Dermatol Venereol 2015;142(8–9):476–82. [CrossRef]
[Pubmed]

3.
Degrugillier-Chopinet C, Bisdorff-Bresson A, Laurian C, et al. Role of duplex Doppler for superficial “angiomas”. [Article in French]. J Mal Vasc 2011;36(6):348–54. [CrossRef]
[Pubmed]

4.
Kilcline C, Frieden IJ. Infantile hemangiomas: How common are they? A systematic review of the medical literature. Pediatr Dermatol 2008;25(2):168–73. [CrossRef]
[Pubmed]

5.
Drolet BA, Esterly NB, Frieden IJ. Hemangiomas in children. N Engl J Med 1999;341(3):173–81. [CrossRef]
[Pubmed]

6.
Hemangioma Investigator Group; Haggstrom AN, Drolet BA, et al. Prospective study of infantile hemangiomas: Demographic, prenatal, and perinatal characteristics. J Pediatr 2007;150(3):291–4. [CrossRef]
[Pubmed]

7.
Drolet BA, Swanson EA, Frieden IJ; Hemangioma Investigator Group. Infantile hemangiomas: An emerging health issue linked to an increased rate of low birth weight infants. J Pediatr 2008;153(5):712–5, 715.e1. [CrossRef]
[Pubmed]

8.
Haggstrom AN, Lammer EJ, Schneider RA, Marcucio R, Frieden IJ. Patterns of infantile hemangiomas: New clues to hemangioma pathogenesis and embryonic facial development. Pediatrics 2006;117(3):698–703. [CrossRef]
[Pubmed]

9.
Chiller KG, Passaro D, Frieden IJ. Hemangiomas of infancy: Clinical characteristics, morphologic subtypes, and their relationship to race, ethnicity, and sex. Arch Dermatol 2002;138(12):1567–76. [CrossRef]
[Pubmed]

10.
11.
North PE, Waner M, Mizeracki A, Mihm MC Jr. GLUT1: A newly discovered immunohistochemical marker for juvenile hemangiomas. Hum Pathol 2000;31(1):11–22. [CrossRef]
[Pubmed]

12.
Haggstrom AN, Drolet BA, Baselga E, et al. Prospective study of infantile hemangiomas: Clinical characteristics predicting complications and treatment. Pediatrics 2006;118(3):882–7. [CrossRef]
[Pubmed]

13.
14.
Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taïeb A. Propranolol for severe hemangiomas of infancy. N Engl J Med 2008;358(24):2649–51. [CrossRef]
[Pubmed]

15.
Hogeling M, Adams S, Wargon O. A randomized controlled trial of propranolol for infantile hemangiomas. Pediatrics 2011;128(2):e259–66. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Dounia Benaich - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Leila Benbella - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mustapha Azekhmam - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohamed Reda Elouchi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Abderrahim Elktaibi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohamed Allaoui - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hafsa Chahdi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Amal Damiri - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohamed Amine Essaoudi - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohammed Oukabli - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Dounia Benaich et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.